For decades, the understanding and treatment of inguinal hernias have relied on approaches that failed to fully respect both the physiology of the abdominal wall and the pathogenesis of the disease. Through extensive research and clinical investigation, Prof. Giuseppe Amato has uncovered new insights into the genesis of hernia protrusions, paving the way for a groundbreaking, biologically coherent approach to hernia repair.
A New Vision: The Role of Dynamic Regenerative Scaffolds
Traditional hernia repair methods primarily focus on covering the defect with a flat mesh, leaving the defect patent and neglecting the biological mechanisms responsible for hernia formation. Prof. Amato’s research has led to the development of an innovative therapeutic paradigm: the use of dynamic regenerative scaffolds, which not only provide mechanical support in a fixation-free fashion but also actively stimulate tissue regeneration, addressing the degenerative origin of hernia disease.
ProFlor: a breakthrough in inguinal hernia repair
The first breakthrough in this field was ProFlor, a dynamic scaffold designed to fully integrate with the abdominal wall and promote natural healing. Specifically developed for inguinal hernioplasty, ProFlor offers key advantages:
- Physiological Repair: Unlike static meshes, ProFlor completely and fixation-free obliterates the hernia defect, moving in sync with surrounding muscles to ensure seamless integration.
- Regenerative Action: The continuous movement of the scaffold stimulates muscle, nerve, and vascular growth, restoring the structural and functional integrity of the abdominal wall.
- Permanent and Secure: The material remains indefinitely in place, overcoming the limitations of absorbable meshes that risk losing effectiveness over time.
Minimally Invasive: ProFlor allows for a faster and simpler mini-invasive hernia repair, significantly reducing postoperative pain, complications, and recovery time. Thanks to its fixation-free delivery and probiotic biological response, it virtually eliminates the risk of chronic pain.
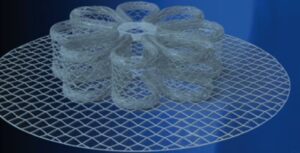
The multilamellar design of the 3D scaffold ProFlor

A 40 mm 3D dynamic scaffold ProFlor, evidently squeezed within the internal ring, obliterates an indirect inguinal hernia defect
The treatment concept for inguinal hernia repair with the 3D dynamic regenerative scaffold ProFlor: the videos show the revolutionary features of the device
https://youtu.be/bB4wPwfIhsE
The ProFlor technique for inguinal hernia repair: open and laparoscopic
https://youtu.be/OKV-fglkBN
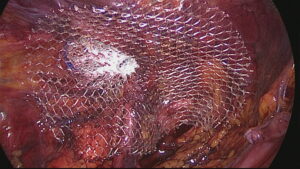
Laparoscopic image of a 40 mm sized dynamic scaffold ProFlor-E positioned into the internal inguinal ring and fully obliterating an indirect hernia defect. The flat portion of the scaffold covers the remaining posterior surface of the groin.
Tissue regeneration following hernia repair with the 3D scaffold ProFlor
The 3D dynamic structure of the ProFlor scaffold permanently obliterates the hernia defect, contracts and relaxes in compliance with the muscular structures of the groin. Due to its continuous movements, ProFlor acts as a regenerative scaffold for the development of new tissue components of the groin, re-establishing the inguinal barrier made of dense, viable and well vascularized tissue. The dynamic scaffold does not shrink, does not cause discomfort and postoperative pain is sharply reduced allowing the return to normal activities within few days postop.
Biologic response: 3D dynamic scaffold ProFlor vs conventional hernia meshes.
In terms of biologic response, the difference between the 3D dynamic scaffold ProFlor and the conventional meshes is noteworthy. Conventional meshes after few weeks start to produce a fibrous, hard, irregular and inelastic scar that leads to shrinkage and surface reduction of the prosthesis. This stiff scar plate, very similar to a foreign body reaction, rubbing on the inguinal floor can cause a frustrating discomfort, often complained by patients even years after surgery. The uncontrolled ingrowth of the hard scar plate, typical of conventional prostheses, is also reputed to be one of the causes of chronic pain, an event that can upset life of patients. To evaluate the differences in tissue incorporation between the two types of devices, conventional static and the 3D dynamic scaffold, Prof. Amato carried out a comparative scientific research on the biological response of the two devices in the short, medium and long-term. This scientific experience showed a manifest superiority in biologic response of the 3D dynamic scaffold ProFlor compared to conventional static meshes. The comparative scientific research demonstrated that over time the conventional flat mesh becomes a mixture of stiff scar amalgamated with amorphous synthetic material. On the contrary, the 3D dynamic scaffold ProFlor is incorporated by a well-vascularized fleshy mass that fully overwhelm its fabric, which is no more recognizable.
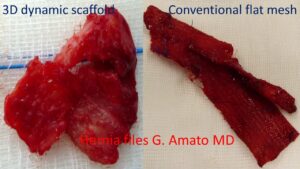
The difference of the biological response after 8 months post implantation between the 3D dynamic scaffold ProFlor, incorporated by fleshy tissue, and a conventional flat hernia mesh, deformed by a rigid scar tissue, is significant.
In the photo here on the side, the difference between the two hernia devices few months postoperative is evident. The picture shows a biopsy of the 3D dynamic scaffold and a conventional static mesh explanted for recurrence. The structure of the 3D dynamic scaffold is no longer recognizable because incorporated by a well-vascularized fleshy tissue. The other picture shows an irregularly folded conventional static mesh turned into a hardened piece of scar plate. The difference is remarkable: viable fleshy structure against a piece of hard cloth!
Quality of regenerated tissue within the structure of the 3D scaffold ProFlor
- After 3 months absence of inflammatory reaction
- Newly formed mature muscle fibers
- Plenty of nerves complete in all constituents
- Well-structured veins and arteries
- Soft and well hydrated connective
For those wishing to deepen the subject, a series of scientific articles related to these researches have been published in high ranked international scientific journals. Among the published reports, the following papers clearly summarize the regenerative features of the 3D scaffold ProFlor:
- Biologic response of inguinal hernia prosthetics: a comparative study of conventional static meshes versus 3D dynamic implants. Artif Organs. 2015 Jan;39(1)
- Neomyogenesis in 3D dynamic responsive prosthesis for inguinal hernia repair. Artif Organs. 2018 Dec;42(12):1216-1223
- Neo-nervegenesis in 3D dynamic responsive implant for inguinal hernia repair. Qualitative study. International Journal of Surgery Volume 76, April 2020, Pages 114-119
- Enhanced angiogenesis in the 3D dynamic responsive implant for inguinal hernia repair ProFlor Artificial Organs. 2021;45:933–942.
- A regenerative 3D scaffold for inguinal hernia repair. MR imaging and histological cross evidence. Qualitative study International Journal of Surgery 2021, 96, 106170
- Dynamic Responsive Inguinal Scaffold Activates Myogenic Growth Factors Finalizing the Regeneration of the Herniated Groin. J Funct Biomater. 2022 Nov 18;13(4):253
- Physiologic Cyclical Load on Inguinal Hernia Scaffold ProFlor Turns Biological Response into Tissue Regeneration. Biology, 2023, 12(3), 434
The Evolution: The Stenting & Shielding Hernia System
Building upon the groundbreaking innovation of ProFlor, Prof. Amato has developed the Stenting & Shielding (S&S) Hernia System, a next-generation dynamic scaffold that revolutionizes the treatment of most abdominal hernia types.
Made of polypropylene based TPE material, in addition to incorporating ProFlor’s key advantages—Fixation-Free Physiological Repair and Dynamic Regenerative Action—the S&S Hernia System introduces:
- A Trauma- and Dissection-Free Approach: The procedure eliminates the need for tissue trauma and dissection, ensuring a gentler, more patient-friendly repair.
- An Ultra-Fast, Simplified Surgical Procedure: The implantation takes just seconds, dramatically simplifying hernia repair while maintaining high safety and efficacy standards.
This video features the Stenting & Shielding Hernia System: https://youtu.be/DlRnSENg5sU
Thanks to its unprecedented procedural simplicity, the S&S Hernia System allows hernia repair to be performed in all clinical settings, including outpatient and ambulatory surgery. The short learning curve ensures that surgeons of all experience levels can quickly adopt the technique, leading to a dramatic reduction in intra- and post-operative complications, as well as instant patient recovery and immediate return to daily activities.

The Stenting & Shielding Hernia System in deployed mode (frontal view)
Scientific Validation & Path to Market
The S&S Hernia System has successfully passed the preclinical phase following an extensive long-term experimental trial on a porcine model. The results of this groundbreaking study, including:
- Surgical outcomes,
- Histological evidence of multi-tissue regeneration, and
- Immunohistochemical proof of growth factor activation,
have been submitted for publication in leading scientific journals.
Now, the S&S Hernia System Project is entering a crucial stage: financial funding and industrial development to bring this revolutionary technology to patients worldwide.
A Paradigm Shift in Hernia Surgery
The discoveries of Prof. Amato mark a fundamental shift in hernia treatment—moving from a passive, overlay-based approach to an active, regenerative solution. By addressing the underlying physiological and pathogenetic mechanisms of hernia formation, the S&S Hernia System offers a safer, more effective, and longer-lasting treatment—ushering in a new era of biologically coherent hernia repair.
OTHER INNOVATIVE SOLUTIONS DEVELOPED BY PROF. AMATO FOR THE TREATMENT OF VENTRAL AND INCISIONAL HERNIAS
Prof. Amato also invented the tentacle shaped implant for the treatment of 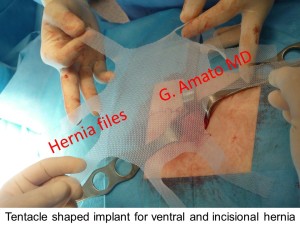 abdominal wall hernias (incisional, umbilical, epigastric and Spigelian hernias). The related surgical technique allows a fixation free surgical procedure for the treatment of these widespread pathologies. Small skin incisions, minimized surgical trauma and sharply reduced postoperative complications are the highpoints of the surgical technique. This is possible thanks to the proprietary design of the prosthesis whose elongated straps at the edges of the implant, inserted through the abdominal wall musculature, allow a permanent fixation free positioning of the implant, using the principle of tissue friction.
abdominal wall hernias (incisional, umbilical, epigastric and Spigelian hernias). The related surgical technique allows a fixation free surgical procedure for the treatment of these widespread pathologies. Small skin incisions, minimized surgical trauma and sharply reduced postoperative complications are the highpoints of the surgical technique. This is possible thanks to the proprietary design of the prosthesis whose elongated straps at the edges of the implant, inserted through the abdominal wall musculature, allow a permanent fixation free positioning of the implant, using the principle of tissue friction.
The modern prosthetic devices and the innovative surgical techniques developed by Prof. Amato allowed for significant decrease of postoperative complications. These techniques have been scientifically validated by numerous articles published in the most important scientific journals.
- Prosthetic stap system for simplified ventral hernia repair: results of a porcine experimental model. Hernia 2010;14:389-95
- A new shape of mesh to simplify and standardize the implantation procedure in ventral hernia repair. Hernia 2010;14:S-43
- Fixation free open ventral hernia repair using a new mesh with integrated placement straps. Hernia 2011;15:S21
- New mesh shape and improved implantation procedure to simplify and standardize open ventral hernia repair. A preliminary report. Hernia 2011;5:659–665
- Fixation free prosthetic repair of large umbilical hernia granting a broad defect overlap. Hernia 2012;16: Sl43-S240
- Fixation free incisional hernia repair with a newly designed mesh with integrated bands. Hernia 2012;16 (Suppl 1): 569-572
- Fixation free prosthetic repair of large umbilical hernia Hernia (2013) 17 (Suppl 2): S1-S26
- Long-term results of fixation free incisional hernia repair using a tentacle shaped implant. Surg. Technol. Int. 2017 Jul 25;30:175-181.
- Fixation free incisional hernia repair in the elderly: our experience with a tentacle-shaped implant. Aging clinical experimental research. Aging Clin. Exp. Res.2017 Feb;29(Suppl 1):173-177
- Long-term results of fixation-free incisional hernia repair with a tentacle-shaped implant. Hernia (2018) 22 (Suppl 1):S115
- Tentacle‑shaped mesh for fixation‑free repair of umbilical hernias. Hernia. 2019 Aug;23(4):801-807
- Fixation-free incisional hernia repair with tentacle-shaped implant: The results of a long-term follow up. Hernia (2019) 23 (Suppl 2):S240
- Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap Journal of Clinical Medicine, 2023, 12(12), 3866